“Lazy eye” is the common term for amblyopia, a condition where one eye does not develop normal vision during childhood. Despite the name, there’s nothing lazy about the eye itself – it’s actually a problem with how the brain and eye work together.
In amblyopia, the brain starts to favour one eye over the other. Over time, it pays less attention to the weaker eye, and vision in that eye doesn’t develop as it should. If left untreated, this reduced vision can become permanent.
What Causes Amblyopia?
Amblyopia usually develops in early childhood and can be caused by:
A significant difference in prescription between the eyes (one eye may be much more long- or short-sighted than the other)
An eye turn (strabismus), where the eyes are not aligned
Anything that blocks clear vision in one eye during early life, such as a cataract or droopy eyelid
Because children often don’t realise they’re seeing poorly in one eye, amblyopia can easily go unnoticed without a proper eye examination.
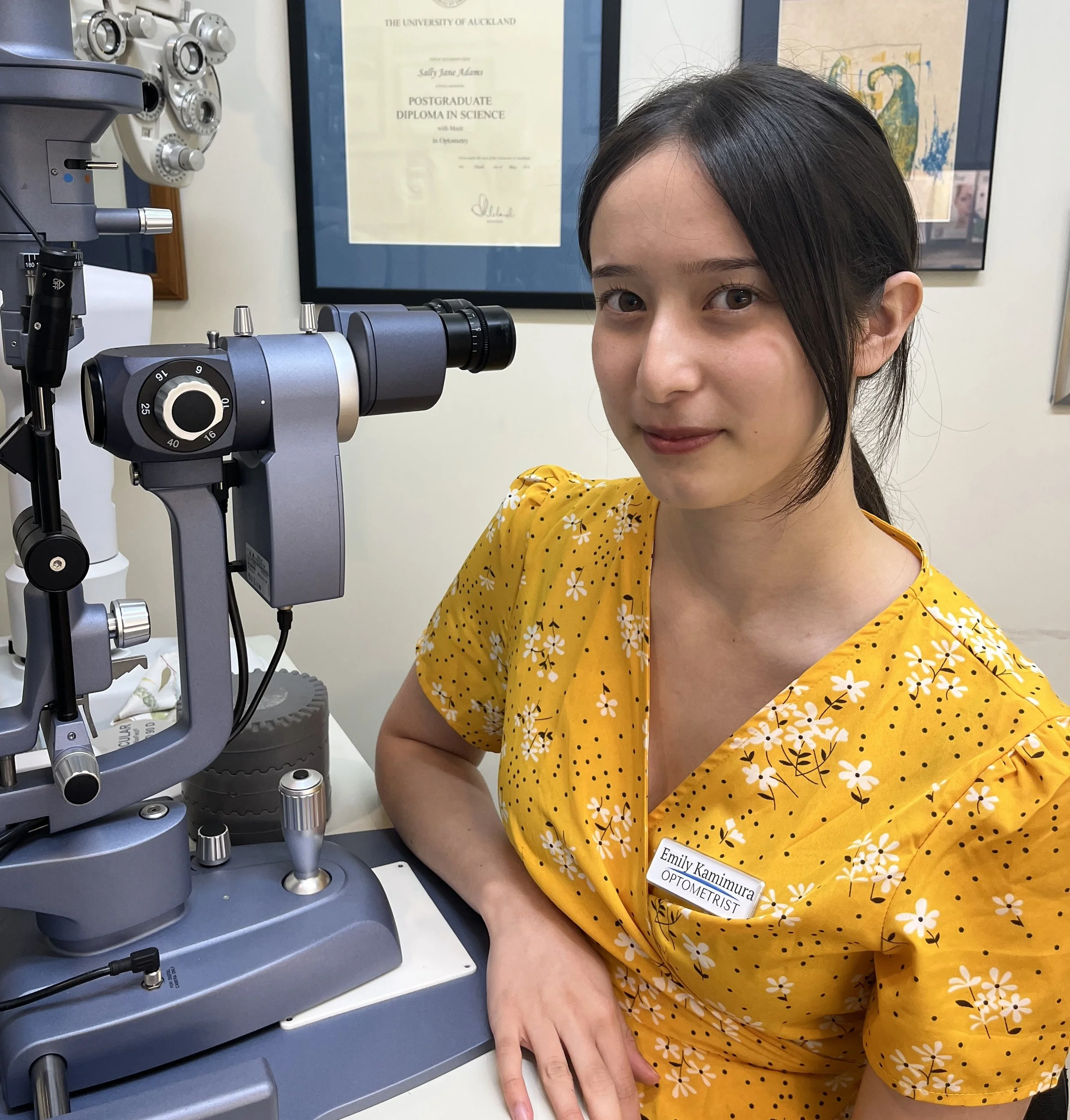
The Role of Optometrists in Children’s Eye Care
Early detection is key. Optometrists play a crucial role in identifying and managing amblyopia, often well before parents notice any signs.
Management may include:
Prescribing glasses to ensure each eye has the clearest vision possible
Monitoring visual development over time
The good news is that amblyopia is most effectively treated in childhood, while the visual system is still developing. So eye examinations for children are important, even if there are no obvious concerns.
What About Amblyopia in Adults?
In adulthood, amblyopia is usually stable. While glasses can optimise vision, they cannot fully correct amblyopia once visual development is complete. This can be disappointing to hear, but there are still important reasons for ongoing eye care.
In amblyopia, there will be a ‘good eye’, which is delivering all the detail vision. This makes eye safety especially important. Protective eyewear for work, sport, and hobbies can help reduce the risk of injury to the better-seeing eye.
Routine eye examinations also remain essential to monitor overall eye health and detect conditions such as glaucoma or macular disease early.
In Summary
A lazy eye is not something to ignore. Early eye checks can make a lifelong difference, whether it’s identifying amblyopia in children or protecting vision in adulthood, regular eye care matters.
If you have concerns about your child’s vision – or your own – an eye examination is the best place to start.